Introduction
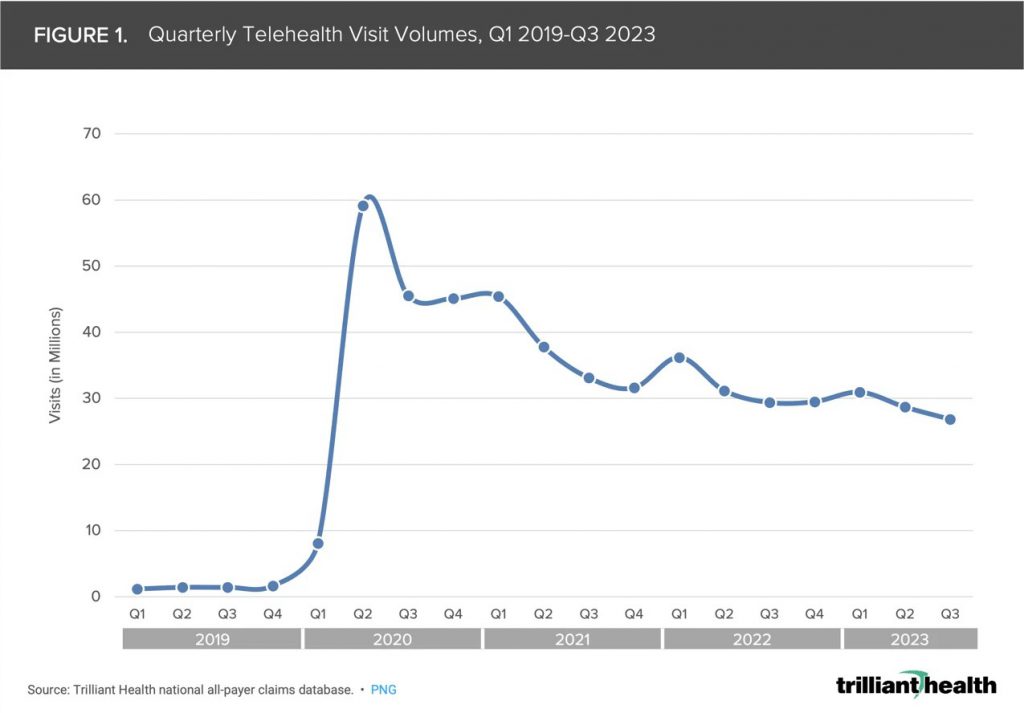
While access to virtual healthcare platforms has been on the rise in recent years, the impact of COVID-19 has accelerated that trend, encouraged by restrictions on office visits and in some instances, reduced or zero insurance copays required by healthcare systems. Patients are realizing more convenient access to healthcare, while avoiding the need to interact with other sick patients, leading to higher satisfaction and loyalty. Providers can better manage privacy concerns and missed appointments, while still scheduling in person visits where most appropriate, thus leading to greater efficiency and satisfaction. The healthcare network is able to expand access into the community, and work toward improved quality measures and outcomes. However, Medicare restrictions and private insurance coverage has not always caught up to these changes, and are still adjusting their administrative policies.
As defined by the American Academy of Family Physicians, “telemedicine” is clinical services delivered by a physician at a remote location, while “telehealth” includes broader scope of remote non-clinical services such as training and patient education. Telemedicine includes delivering care to patient within their current system via real-time communication, but could also utilize remote clinical services of a specialist brought onto the care team, which may occur at small, rural hospitals. This article will primarily focus on virtual care within a pre-existing patient / provider relationship.
A recent report from McKinsey and Company projects a rise in telehealth services could eventually result in a shift of $250 billion of current US healthcare costs. This could eventually include 20% of ED visits and 24% of outpatient office visits. Increased utilization of wearable devices to monitor pre-existing health conditions may also contribute to these trends.
According to the AMA Telehealth Implementation Playbook and the American Academy of Family Physicians, telemedicine is most appropriate for simple and low-risk diagnoses requiring a prescription (i.e. colds and flu, UTI’s), follow up and recurring care to manage chronic conditions, behavioral health counseling and medication management, other routine appointments, and for people with transportation difficulties. If these projections are realized, healthcare planning will certainly need to consider and accommodate these impacts.
Planning Considerations
The 2018 edition of Guidelines for Design and Construction of Outpatient Facilities greatly expanded on the recommendations for design of spaces devoted to telemedicine services. However, they state in the Appendix that, “The requirements in this section are not intended to apply to virtual visits that do not require a physical examination of the patient or visits that originate from a physician’s or patient’s home.” Regardless, their recommendations are useful for all types of virtual care, as they speak to the environmental characteristics suggested for effective delivery of care in a remote setting.
Telemedicine can also take two paths: consultation with the patient’s primary care provider, or by a physician or other healthcare professional dedicated to virtual appointments. In either instance, care is not being delivered in a physical office, and therefore, program needs are impacted. These are some areas to consider when a portion of the patient volume is diverted:
- Are fewer parking spaces needed?
- Waiting room size: does a smaller in-person caseload reduce delays in the waiting room, or will social distancing concerns just spread-out waiting patients?
- Exam rooms – review and respond to daily patient volumes and trends, rather than basing need on number of providers or past experience.
- How are changes in workflow accommodated, such as access to electronic medical records by a physician other than the patient’s care provider? Are fewer nursing and support staff needed?
- How will virtual visits impact secondary diversions from Urgent Care and ED?
Program Needs

It is critical that spaces designed to provide telemedicine services does not distract or compromise the provider’s ability to provide the same high-quality level of care as an in-person encounter. Not only does the provider need to project a professional image in their appearance and body language, but the environment where a virtual encounter takes place needs to be carefully considered. First, will the space be located where provider can easily access without disrupting the daily flow of activities, and still maintain a sufficient level of privacy and focus? If such a space is being retrofit in an existing clinic, a consultation space may be more suitable than an exam room or doctor’s private office.
The technology for virtual meeting platforms is evolving quickly, and so infrastructure must be designed for flexibility. Patients may be using an app on their phone or other portable device, and bandwidth limitations should be considered so that calls are not lost in the middle of the visit. Patient confidentiality also means concerns regarding cybersecurity must be addressed.
Once space is identified, appropriate lighting and acoustics need to enable patient to communicate without distractions or concerns over confidentiality. The background should be a neutral, non-glossy color with minimal visual clutter. Camera should be positioned at eye level to encourage personal interaction.
Conclusion
Although the arrival of telemedicine has been anticipated for several years now, the impact of COVID-19 may encourage patients to embrace virtual care permanently. While still evolving, it can never fully replace the traditional care model. The ability to address minor or ongoing care issues remotely will allow providers to focus their efforts, and identify early on when more personal intervention is needed.
 About the Author: Michael Schaefer, AIA, NCARB, CCCA, LEED AP
About the Author: Michael Schaefer, AIA, NCARB, CCCA, LEED AP
Michael has been with PRA since 1994, and since then worked in various studios but specializes in
Healthcare. Michael’s passion for creating healthy living environments is incomparable to anyone
else. He feels a large responsibility to design spaces that not only assists healthcare providers but
comforts the patients and families in need of care. He believes the work he does is highly rewarding
when he can create an environment that makes patients and caregivers feel safe, calm, and hopeful.
He also enjoys working with all his clients because their knowledge and passion is infectious, which
motivates him to always go the extra mile.