By LAK Group
For many years, organizational learning was treated as an event: classrooms, workshops, multi-hour webinars, and long e-learning modules. People left their day-to-day responsibilities, attended a program, and then tried, often with mixed success, to apply what they had learned back on the job. Valuable? Yes. But in today’s faster, more complex environment, this model on its own is no longer enough.
That’s where the idea of learning in the flow of work comes in. Popularized by Josh Bersin, the concept is simple but powerful: instead of pulling employees away from their work to learn, we design learning so it happens while they are working, at the moment of need, in the context of real tasks, and in ways that are quick, relevant, and easy to access.
What Do We Mean by “Learning in the Flow of Work”?
Learning in the flow of work is about giving people “just enough” learning, “just in time,” so they can use it immediately. Rather than a separate activity reserved for training days, development becomes a natural part of everyday execution.
In practice, this can look like a manager pulling up a short conversation guide before delivering difficult feedback, a leader using an AI-enabled tool to rehearse a tough conversation, or a team accessing a quick decision framework while working through a complex problem. The common thread is that learning is embedded in real work, not abstracted away from it.
This approach matters because modern work rarely slows down. Organizations are navigating constant change, new technologies, shifting customer expectations, and evolving employee needs. Teams have limited capacity to step out for lengthy programs, but they still need to grow. Learning in the flow of work helps close the gap between “I know this” and “I actually used this,” which is where most traditional training falls short.
Why Learning in the Flow of Work Matters Now
Three realities make this approach especially important today. First, work is fast-moving. Business priorities shift quickly, and leaders often feel they cannot afford to take people out of the operation for large chunks of time. Second, work is increasingly complex and distributed. Hybrid and remote teams, new tools, and cross-functional collaboration all create scenarios in which the “right way” to act is highly contextual and constantly evolving. Finally, organizations are under pressure to show real impact from learning and development investments. It’s no longer enough to track attendance; stakeholders want to see behavior change and business results.
By embedding learning into everyday workflows, organizations increase the likelihood that new ideas are applied immediately, reinforced over time, and connected directly to performance. Research has long shown that people retain more when they can practice and apply new skills in context, not just hear about them in theory.
What Learning in the Flow of Work Looks Like
A common misconception is that learning in the flow of work requires a wholesale redesign of all programs. In reality, it often starts with small, practical shifts.
Some organizations begin by creating job-embedded tools: short guides, checklists, or templates that sit as close as possible to the work itself. For example, a one-page framework for giving feedback, a set of coaching questions for one-on-one meetings, or a quick reference for handling difficult customer situations. When these resources are easy to find and simple to use, employees are far more likely to apply them.
Others focus on integrating real-time coaching and feedback into existing rhythms. Instead of waiting for annual programs, leaders and coaches work with people on live challenges: preparing for a specific conversation, debriefing a key meeting, or reflecting on a recent decision. This turns real work into the primary learning lab.
Short, focused “micro-learning” experiences also play a role. These might be five- to ten-minute modules or brief videos that are timed to upcoming tasks, “before your next 1:1,” “before your next client presentation,” or “before you run that performance discussion.” The key is that content is targeted, practical, and immediately usable.
Increasingly, technology is a critical enabler. Learning platforms can integrate with calendars, collaboration tools, and performance systems to surface relevant resources at the right time. Generative AI can help leaders draft feedback, rehearse conversations, and explore “what if” scenarios in a safe environment, providing low-risk practice opportunities that complement human coaching rather than replacing it.
The Crucial Role of Leaders
No matter how good the tools or content are, learning in the flow of work succeeds or fails based on leadership behavior.
When leaders treat learning as a separate, optional activity, employees will do the same. But when leaders consistently pause to ask questions like “What did we learn from this?” or “How will we handle this differently next time?” they send a powerful signal that reflection is part of the job, not a luxury.
Leaders who share their own learning openly, admitting mistakes, naming insights, and modeling new behaviors, make it safer for others to do the same. Over time, this builds a culture in which learning is not an event but an ongoing practice woven into meetings, decisions, and day-to-day interactions.
Getting Started: A Practical Approach
The good news is that you do not need a massive change program to begin moving toward learning in the flow of work. A practical way to start is to choose one critical moment in your organization’s work and focus there. It might be onboarding, performance conversations, sales meetings, or project kick-offs, any situation where better preparation and reflection would clearly improve outcomes.
From there, ask where people feel stuck or unprepared and design one or two simple supports: a guide, a short learning resource, a targeted coaching touchpoint, or an AI-enabled tool that offers structure and language in the moment of need. Pilot with a small population, gather feedback on whether the support helped “in the moment,” and refine from there. Over time, you can add more moments and more layers, gradually building a learning ecosystem that is truly integrated into work.
Call to Action: Partner with LAK Group
At LAK Group, we help organizations move from event-based learning to integrated, real-time development by combining leadership coaching, talent assessment, and modern learning design. Our work is grounded in helping leaders and teams learn while they work, through coaching in the flow of real challenges, AI-enabled practice experiences, and programs that are tightly connected to your strategy.
If you’re ready to explore how learning in the flow of work could look in your organization, starting with a focused pilot or a leadership cohort, we’d be glad to talk.
Let’s design a learning experience that meets your people where they work. Contact LAK Group to schedule a conversation about learning in the flow of work and what it could mean for your leaders, teams, and business.
References
- Bersin, J. (2018). A New Paradigm For Corporate Training: Learning In The Flow Of Work.
- Center for Creative Leadership. (n.d.). The 70-20-10 Rule for Leadership Development – emphasizing the importance of on-the-job experiences in driving growth.
- Deloitte Human Capital Trends. (Various years). Findings consistently highlight the need for continuous, integrated learning in response to rapid organizational change.


 About the Author: Michael Schaefer, AIA, NCARB, CCCA, LEED AP
About the Author: Michael Schaefer, AIA, NCARB, CCCA, LEED AP
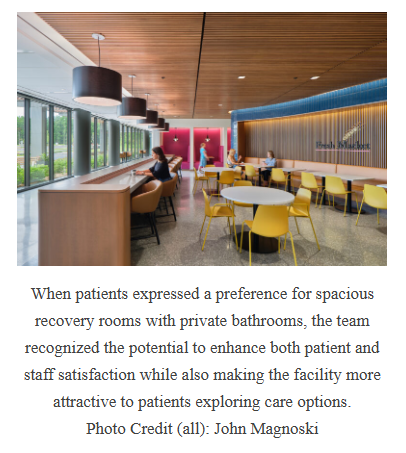 Take, for instance, the challenge of diverging stakeholder needs. Physicians, as primary users, often emphasize efficiency, valuing workflows that allow them to treat as many patients as possible in a streamlined manner. On the other hand, patients prioritize comfort, privacy and dignity. Investors focus on the bottom line, seeking a balance between upfront costs and long-term returns.
Take, for instance, the challenge of diverging stakeholder needs. Physicians, as primary users, often emphasize efficiency, valuing workflows that allow them to treat as many patients as possible in a streamlined manner. On the other hand, patients prioritize comfort, privacy and dignity. Investors focus on the bottom line, seeking a balance between upfront costs and long-term returns. With operational strategies in place, ownership structures further shape design considerations. Single-owner systems, such as hospital-led ASCs, often emphasize branding and quality (which can inflate costs), while joint ventures introduce competing priorities between clinical goals and financial imperatives. Modular designs that are easily expandable keep building size and costs low for initial market investments but allow rapid expansion as volumes and market share increase. For example, a new market facility’s initial four operating rooms could adapt to different configurations, supporting immediate operational needs and future growth. This flexibility was particularly valuable for ownership groups focused on scaling operations quickly. Projects that prioritized adaptive layouts allowed for rapid reconfigurations, helping facilities remain competitive in dynamic markets.
With operational strategies in place, ownership structures further shape design considerations. Single-owner systems, such as hospital-led ASCs, often emphasize branding and quality (which can inflate costs), while joint ventures introduce competing priorities between clinical goals and financial imperatives. Modular designs that are easily expandable keep building size and costs low for initial market investments but allow rapid expansion as volumes and market share increase. For example, a new market facility’s initial four operating rooms could adapt to different configurations, supporting immediate operational needs and future growth. This flexibility was particularly valuable for ownership groups focused on scaling operations quickly. Projects that prioritized adaptive layouts allowed for rapid reconfigurations, helping facilities remain competitive in dynamic markets.